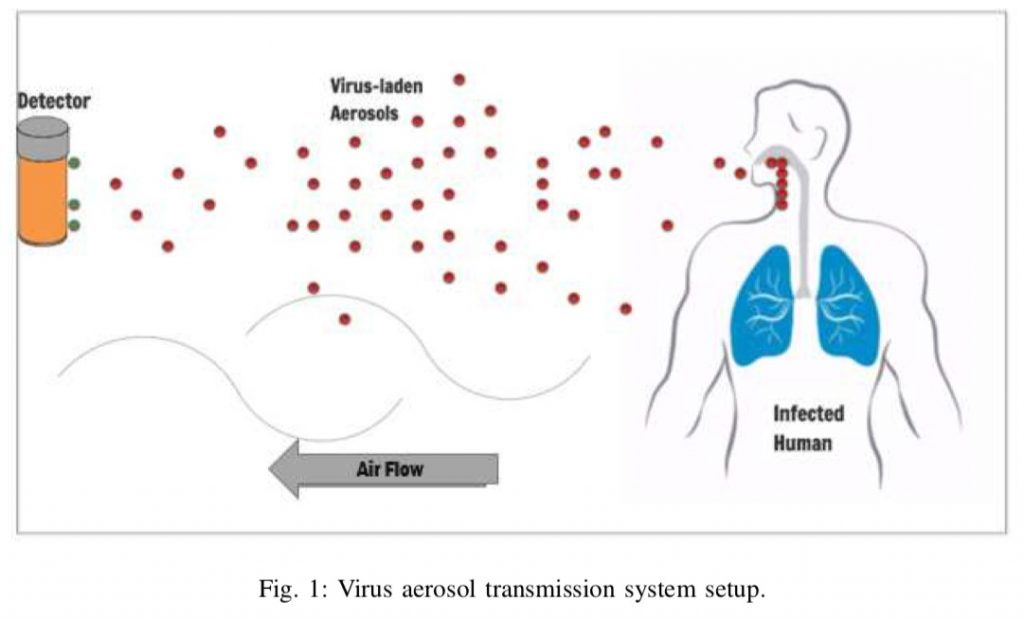
What many scientists have been saying for months ever since the spread of Corona Virus is the virus lingers in the air indoors, infecting those nearby.
This has come true with the findings that coronavirus giving rise to frightening clusters of infection that increasingly attack new victims worldwide, in bars and restaurants, offices, markets and casinos
The World Health Organisation (WHO) has long held that the coronavirus is spread primarily by large respiratory droplets that, once expelled by infected people in coughs and sneezes, fall quickly to the floor.
But in an open letter to the WHO, 239 scientists in 32 countries have outlined the evidence showing that smaller particles can infect people and are calling for the agency to revise its recommendations. The researchers plan to publish their letter in a scientific journal.
Even in its latest update on the coronavirus, released June 29, the WHO said airborne transmission of the virus is possible only after medical procedures that produce aerosols, or droplets smaller than 5 microns. (A micron is equal to 1 millionth of a metre.)
Proper ventilation and N95 masks are of concern only in those circumstances, according to the WHO.
[splco_spacer]
[splco_spacer]
Instead, its infection control guidance, before and during this pandemic, has heavily promoted the importance of handwashing as a primary prevention strategy, even though there is limited evidence for transmission of the virus from surfaces. (The Centres for Disease Control and Prevention now says surfaces are likely to play only a minor role.)
Dr Benedetta Allegranzi, the WHO’s technical lead on infection control, said the evidence for the virus spreading by air was unconvincing.
“Especially in the last couple of months, we have been stating several times that we consider airborne transmission as possible but certainly not supported by solid or even clear evidence,” she said. “There is a strong debate on this.”
But interviews with nearly 20 scientists – including a dozen WHO consultants and several members of the committee that crafted the guidance – and internal e-mails paint a picture of an organisation that, despite good intentions, is out of step with science.
Whether carried aloft by large droplets that zoom through the air after a sneeze, or by much smaller exhaled droplets that may glide the length of a room, these experts said, the coronavirus is borne through air and can infect people when inhaled.
Most of these experts sympathised with the WHO’s growing portfolio and shrinking budget, and noted the tricky political relationships it has to manage, especially with the United States and China. They praised WHO staff for holding daily briefings and tirelessly answering questions about the pandemic.
But the infection prevention and control committee in particular, experts said, is bound by a rigid and overly medicalised view of scientific evidence, is slow and risk-averse in updating its guidance and allows a few conservative voices to shout down dissent.
“They’ll die defending their view,” said one longstanding WHO consultant, who did not wish to be identified because of her continuing work for the organisation. Even its staunchest supporters said the committee should diversify its expertise and relax its criteria for proof, especially in a fast-moving outbreak.
“I do get frustrated about the issues of airflow and sizing of particles, absolutely,” said Dr Mary-Louise McLaws, a committee member and epidemiologist at the University of New South Wales in Sydney.
“If we started revisiting airflow, we would have to be prepared to change a lot of what we do,” she said. “I think it’s a good idea, a very good idea, but it will cause an enormous shudder through the infection control society.”
Dr Lidia Morawska, the group’s leader and a long-time WHO consultant and others pointed to several incidents that indicate airborne transmission of the virus, particularly in poorly ventilated and crowded indoor spaces.
They said the WHO was making an artificial distinction between tiny aerosols and larger droplets, even though infected people produce both.
“We’ve known since 1946 that coughing and talking generate aerosols,” said Dr Linsey Marr, an expert in airborne transmission of viruses at Virginia Tech.
Scientists have not been able to grow the coronavirus from aerosols in the lab. But that doesn’t mean aerosols are not infective, Dr Marr said: Most of the samples in those experiments have come from hospital rooms with good air flow that would dilute viral levels.
In most buildings, she said, “the air-exchange rate is usually much lower, allowing virus to accumulate in the air and pose a greater risk.”
The WHO also is relying on a dated definition of airborne transmission, Dr Marr said. The agency believes an airborne pathogen, like the measles virus, has to be highly infectious and to travel long distances.
Dr Marr and others said the coronavirus seemed to be most infectious when people were in prolonged contact at close range, especially indoors, and even more so in superspreader events – exactly what scientists would expect from aerosol transmission.
If airborne transmission is a significant factor in the pandemic, especially in crowded spaces with poor ventilation, the consequences for containment will be significant.
Masks may be needed indoors, even in socially distant settings. Healthcare workers may need N95 masks that filter out even the smallest respiratory droplets as they care for coronavirus patients.
Ventilation systems in schools, nursing homes, residences and businesses may need to minimise recirculating air and add powerful new filters.
Ultraviolet lights may be needed to kill viral particles floating in tiny droplets indoors.