[splco_heading size=”15″ align=”left” margin=”30″]The Coronavirus infection is increasingly spreading among healthcare professionals at various places across India and forcing them to go in quarantine. This has led to a shortage of doctors in many top hospitals in the country. It is also discouraging many others to lead from the front as they are concerned about their own lives and well-being.[/splco_heading]
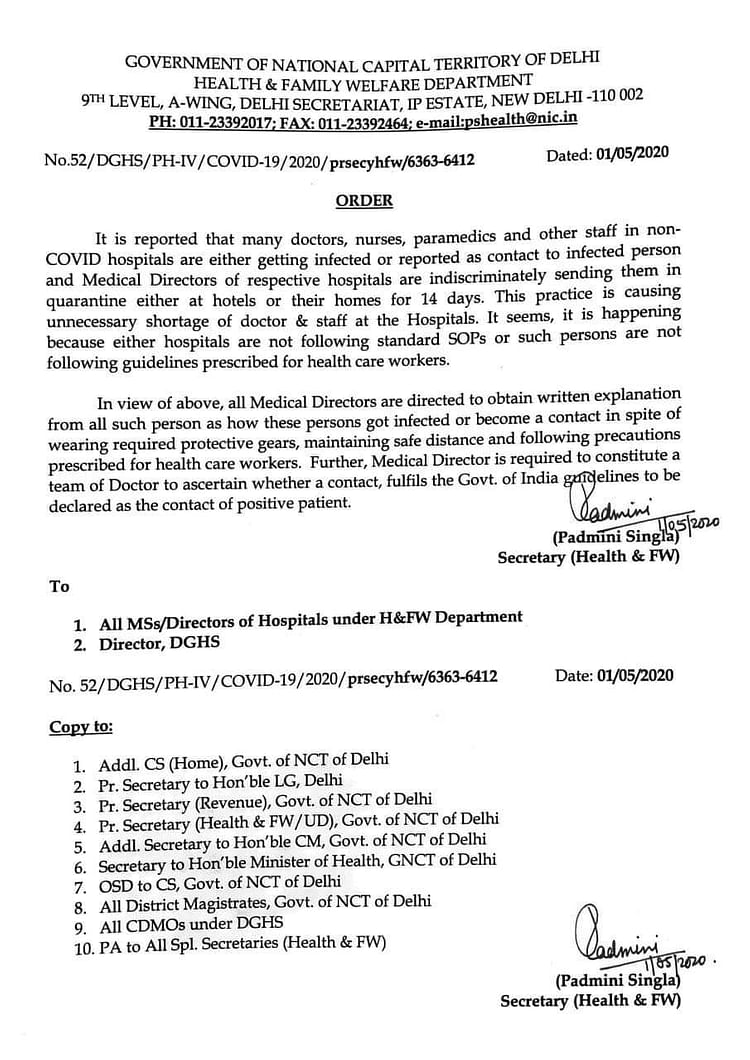
Concerned over rising instances of doctors falling sick, Padmini Singh, Secretary, Health and Family Welfare, Delhi government has asked medical directors of various government hospitals to get written explanation from such doctors, who have tested positive for the virus, asking them how “in spite of wearing required protective gears, maintaining safe distances and following precautions prescribed for healthcare workers, they still contracted the infection.”
However irked by this development and termed it an insensitive move, doctors have opposed it.
Dr Adarsh Pratap Singh, President, Residents’ Doctors Association, AIIMS, New Delhi, says that the current trend is quite worrisome.
Singh has blamed the government for failing to provide basic facilities and services to healthcare professionals in several hospitals.
“Government, health agencies and hospital administration have to focus on these things to prevent such catastrophe to happen with healthcare providers,” Singh says.
Following Center governemnt directive Singh and other doctors have listed below ten demands and asked the government to take urgent steps.
[splco_spacer]

[splco_spacer]
Inadequate and substandard supply of PPE:
In many COVID-19 hospitals, the healthcare professionals don’t have access to complete personal protection equipment (PPE) which make them vulnerable to the infection. In some hospitals, the quality is so inferior that it fails to serve the purpose.
Non-availability of PPE to doctors treating non-COVID patients:
Such patients often bring infection in non-COVID wards unknowingly and infect doctors. Today, PPE is a must for every doctor. As the numbers of hotspots are increasing, so are the asymptomatic COVID-19 positive patients.
Safer accommodation needed for doctors:
Many health workers are at the risk while commuting from home as in many cases they get infected due to community transmission. They need accommodation at safer places, closer to their respective hospitals.
Lesser number of testing:
More testing will isolate more infected people causing a minimum risk to doctors.
Exposure to COVID-19 patients for long:
Since health workers are inadequate in numbers, they have to work for long to attend COVID patients. It leads to more viruses entering into their bodies and making them sick.
Inadequate infection prevention, control training:
Health workers in many districts are poorly trained to handle this infectious disease. A quick training can help them save themselves and others.
Increase in work stress, intensity and anxiety:
Working in a life-threatening environment without proper facilities and care is stressful for health workers. They are de-motivated.
Social ostracism, harassment and assault:
Despite a law to ensure protection to health workers, social ostracism continues unabated. Instead of treating them as warriors, they are seen as a threat and are harassed.
Invest more in healthcare:
It is time the government should realise to invest more in infrastructure and capacity building to fight a pandemic like COVID-19.
Bring private practitioner back to work:
Government healthcare professionals are overburdened because private practitioners have closed their clinics and dispensaries. They should be asked to start working to ease off burden in government hospitals.